The most worrying trend in female healthcare research is the lack of it.
Women (defined here as both female-identifying people, and people with wombs) have always found it much harder than men to have their bodies defined in the medical sphere. Given that histories are recorded and circumstances dictated by men, it’s not surprising that womanhood is ‘othered’ in our self-definition as a species – pushed to the boundaries of experience – but this sense of alienation is particularly prevalent when it comes to our physiognomy.
The female body has long been admired and feared by artists, writers, theologians, and scientists alike. For all recorded history we’ve been seen as boundaryless, apocryphal, excessive, and sinful; capable of divine acts of immaculate conception as well as wild and untameable; connected to the moon and the tide, bleeding and overflowing and seductive.

Though women have been menstruating since before homo sapiens were fully evolved as a species, it wasn’t until the 19th century that scientists linked periods to ovulation. Ancient societies associated periods with witchcraft, postulating that the blood could stop hailstorms, kill crop yields, and cure leprosy, if they wrote about menstruation at all. As late as the 1920s, medical professionals believed periods regulated women’s emotions and tempers, and were disconnected from them physiologically.
Narratives like this place the female form on a pedestal where it can be admired, suspected for its mysterious qualities, and kept in the shadow of ignorance. Centuries on, and the liminal nature of the female body has become so ingrained that even now we do not have a scientific grasp on them.
Many female specific ailments, like endometriosis, polycystic ovary syndrome (PCOS), premenstrual dysphoric disorder (PMDD), and vaginismus are woefully under-researched, with their causes and treatments unknown. Women are constantly misdiagnosed and mistreated by both male and female physicians, and the lack of desire to curb this trend is yet another sign of the taboo around female bodies.
The gender health care gap is both a national and an international issue – whilst healthcare is administered locally, medical research is conducted globally. The problem is inherently one of discourse: as female issues continue to be swept under the rug, unconscious bias will continue to be part of medical training and practicing.
So, if talking and active consciousness is the cure, let’s discuss.
Girl, interrupted
In The Second Sex, Simone de Beauvoir lays out perhaps the best summary of the roots of sexism I’ve ever read: ‘Representation of the world, like the world itself, is the work of men; they describe it from their own point of view, which they confuse with absolute truth.’
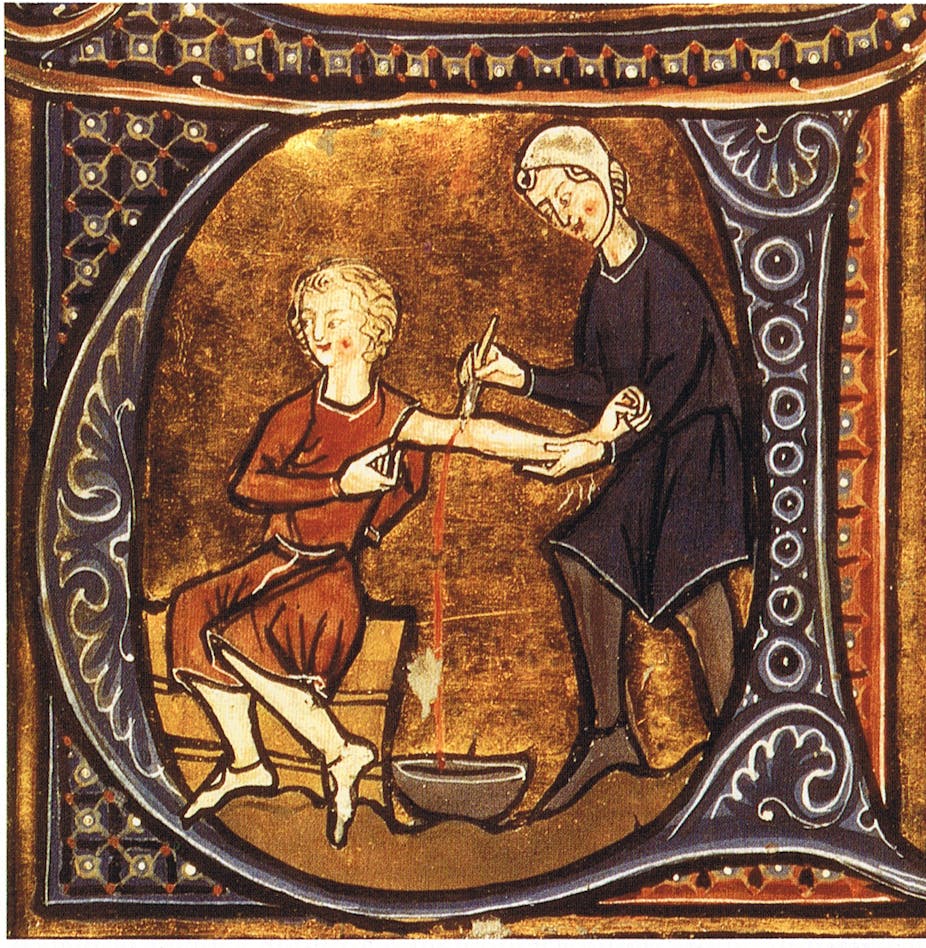
This is entirely true when it comes to medical science. To understand how the male body became the default human construction, we have to go back to the 15th and 16th centuries when biology was first meaningfully applied to humans. Physicians used to employ graverobbers to excavate cadavers or steal them from the gallows for dissection. The corpses they brought back became the basis for the earliest understandings of how we move, bleed, digest food, think, and feel; and, as female hormonal fluctuations were considered too deviant to make consistent calculations, they were, of course, always male. Maleness became the model by which medications were developed, and their effects on people studied.
Centuries later, and that masculinity still seems to be the industry standard. Learning from male bodies is frequently the default in clinical trials today, where subjects are overwhelmingly men – even the standard laboratory mice are male. The Medical Research Council (MRC), which funds and helps coordinate medical research in the UK, has stated that they are yet to produce guidelines on study design relating to the sex or gender of participants.
This is incredibly restrictive to women hoping to access proper medical care, as the only options available to us are functionally potluck.
The range of remedies arbitrarily thrown at ill women throughout history reads like a Doctor Seuss advice column. They were told to swallow toads to ease heavy menstrual flow, had hemp and corn forced up their vaginas to induce labour, and told to marry and bear children early lest their womb (thought by the ancient Greeks to have a mind of its own) dislodge and glide freely about their body.
‘Hysteria’ was a common medical diagnosis for women who displayed all manner of symptoms, ranging from shortness of breath, to fainting, to insomnia, to fluid retention. It was as much a catch-all term for physicians as a form of social control: a bad case of hysteria was attributed to women who had sex outside of marriage, displayed an attraction to the same sex, or violated any of the myriad patriarchal social mores of the time.
Though ‘hysteria’ is no longer a legitimate medical diagnosis, many centuries later there remains a worrying trend of mass invalidation when it comes to women and the healthcare system. Research has found that women are assumed to be both more emotionally volatile, and to have a higher pain threshold, than men. This means that they are far more likely to have their pain reported by doctors as ‘emotional’, ‘psychogenic’, and ‘not real’ according to a seminal 2001 study.
Ohmygods look at the absolute state of this misogyny! 😆
Have constant internal bleeding from #endometriosis for 25y that no doctor, medication, or surgery can cure and then come back with "doing it wrong" when you've understood science facts, kiddo ⭐ https://t.co/JRlJuspDAF
— Miss Lucy #TheBigSnip40 (@TheCurlyLucy) September 1, 2020
Indeed, Women’s bodies are inherently linked with pain – childbirth, PMS, menopause – and the nature of that pain has always been considered vague, shrugged off with the adage that ‘being a woman inherently hurts’. The same 2001 study also revealed that when in pain, men are more likely to be given painkillers, while women are more likely to be given sedatives or antidepressants.
This lack of ability, or even desire, to take women at their word predictably leads to high rates of misdiagnosis and delayed care. A study funded by the British Heart Foundation revealed that women who suffer heart attacks are half as likely as men to receive the recommended medical treatment for cardiovascular issues – for instance, only 15% of female patients were fitted with a stent after a heart attack, compared to 34% of men. This follows other recent research by the BHF which found that over 8,000 women in England and Wales had died of misdiagnosed or untreated heart attacks they’d tried to report over a ten-year period.
In fields as diverse as brain cancer, chronic pain, and dementia, women can take up to seven times longer than male patients to receive a diagnosis. ‘The health gender gap is fed by perceptions of women as being over- emotional and exaggerating the extent of their pain and suffering,’ says women’s health specialist Dr Larisa Corda. ‘In reality, many women under-report symptoms… If they’re not taken seriously when they do see a doctor, it propagates the notion that whatever they’re going through isn’t serious, which can have massive implications.’